What Is An Esophagoscopy?
Last Reviewed: 20th June 2016.
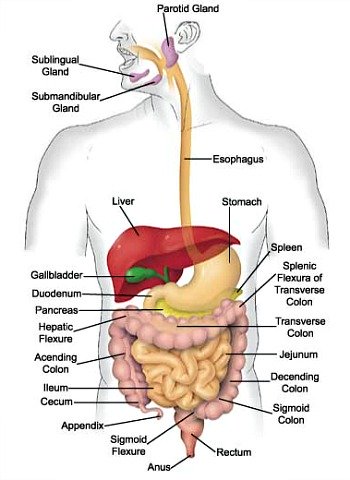
Esophagoscopy is the use of a pen-size tube with a small light source and camera mounted on it, passed through the nose or mouth, down the throat, to directly examine the esophagus. This small light and camera fitted tube is called the esophagoscope or endoscope.
 Esophagoscopy in a 36 year old man showing severe esophagitis (inflammation of the esophagus) from acid reflux.
Esophagoscopy in a 36 year old man showing severe esophagitis (inflammation of the esophagus) from acid reflux.Also called oesophagoscopy in the United Kingdom, this procedure is commonly done to investigate or treat of a number of medical and surgical conditions.
If the endoscope is introduced further down into the stomach and then even further to the duodenum, the procedure is then referred to as an EGD or esophago-gastro-duodenoscopy.
The device on the end of the endoscope creates a display of magnified images on a monitor, which your doctor can watch all the way down the throat to the junction of the oesophagus and stomach, which is called the OG junction. It is unusual to stop an endoscopy just at the esophagus and stomach junction, without looking further down the digestive tract to the duodenum.
Types of Esophagoscopy
The following are the different types of esophagoscopy:
- Flexible Esophagoscopy. This is the use of a flexible endoscope. This means that the pen-size tube fitted with light is bendable and able to navigate and negotiate the bends in the nose or throat. A flexible esophagoscope is often the preferred choice and most commonly used for routine endoscopy of the esophagus. It causes less trauma.
- Rigid Esophagoscopy. This is the use of an inflexible endoscope. This is less used these days.
- Trans-Nasal Esophagoscopy. This refers to the introduction of the endoscope through a nostrils, down the throat rather than through the mouth. Transnasal endoscopy is found to be less painful, brings more of the throat and upper gut to view as well as causes less pulse and blood pressure fluctuation with less gag reflex triggering. It is increasingly becoming the preferred route for esophageal endoscopy. Only a flexible esophageal endoscope can be used to carry out a trans-nasal oesophagoscopy.
- Oral Esophagoscopy. This is the traditional way of passing an esophageal endoscope to take a look at the esophagus. A flexible or rigid oesophagoscope could be used here. The instrument is introduced directly through the opened mouth down the throat and gullet or esophagus. It is more likely to trigger a gag reflex than through the nasal route.
How An Oesophagoscopy Is Performed
Like an EGD or gastroscopy, this procedure is done by a gastroenterologist or another specialist, who is well trained in this regard.
- After you arrive at the doctor’s office, you will be given a gown or sheet and asked to remove your street clothes, and change into the gown or drape.
- You can leave your underwear on.
- You will be taken to a special room equipped with an endoscope and a video monitor, and you will be asked to lie down on the examining table.
- Your doctor will tell you what position in which to arrange yourself.
- In some countries, like the United States, your doctor may give you a sedative and a narcotic pain medication to help you remain comfortable during the procedure. He or she will also spray some numbing spray in your nose or throat, depending upon which way he is entering the esophagus.
- In many countries, only topical anesthetic is considered necessary.
Before the procedure, your doctor will have your entire medical history to study, and will examine the mouth and neck, particularly your thyroid gland, your pharynx, and your teeth. He will check to see if you have enlarged lymph nodes. He will explain the risks, possible complications, benefits, and alternative imaging procedures that might be substituted.
You will be asked to lie on your side, before you receive intravenous sedatives and pain medication, which are given through a vein in your arm. The nurse will clean your arm with an antiseptic before introducing the needle.
After numbing the throat or nostrils, the doctor will gently guide the endoscopic tube through the mouth, pharynx, and into the esophagus. He will be watching the video screen the whole time, so he doesn’t miss any abnormalities.
If there are abnormalities, he will treat them if possible, by doing one of the following things:
- Taking a biopsy specimen from the esophagus to send for analysis under a microscope, with special staining to help identify unusual tissues
- If you have esophageal varices, engorged blood vessels that may hemorrhage, he will place a band around them and they will not receive blood past the band, which will make that tissue die and fall off
- If you, or a child, have swallowed a foreign object that is stuck in the esophagus, the doctor will use a net, forceps, or snares, to retrieve and remove the object.
- If you are bleeding in your esophagus, the doctor can use a special chemical to cauterize the bleeding vessel, or he can place a small clip on the vessel.
- If you have a narrowing of the esophagus, caused by tight tissue growth called strictures, your doctor may inflate a balloon to dilate the area, or he may use an esophageal dilator.
- If you have abnormal tissue that is evident to the naked eye, then your doctor will use a radio-frequency device to destroy the tissue so healthy tissue can regrow in the area.
- He can place a stent to bypass narrowed areas of the esophagus, which may be partially obstructed by a malignant tumor.
- You doctor can give injections, or insert tubes into the esophagus, if needed.
Why Did My Doctor Order An Oesophagoscopy?

Your doctor - family doctor or specialist may order an esophagoscopy to help exam, or take a direct look at the esophagus if he or she suspects that your symptoms may be due to a disorder in the esophagus.
It is usually done as an outpatient, but is sometimes done in emergency situations in the emergency department or in the hospital room.
Some reasons to order an esophagoscopy include:
- Directly visualize the inner wall or lining of the gullet or esophagus to look for a possible change in the anatomy of the esophagus.
- Access the esophagus and take a biopsy from a suspected growth in the esophagus if any was seen previously.
- Reach the esophagus and treat conditions like stopping a bleed in the gullet.
- Reach and remove a foreign body stuck in the esophagus.
- Routine studies to look at your oesophagus is you have a precancerous or cancerous condition.
- To stretch out the oesophagus if you develop strictures frequently.
- If you have swallowed a foreign object and it is stuck in the thin muscular tube that is the oesophagus.
- Evaluation of chest pain that is thought to arise from other sources, not due to a heart problem.
- Evaluation of reflux.
- Heartburn.
- If you have liver disease, your veins in the oesophagus may be very dilated and twisted, and they could begin to hemorrhage, so your doctor will want to watch them and treat them.
- If you have difficulty swallowing (dysphagia).
- If you have pain with swallowing (odynophagia).
- Managing esophageal cancer complications, including placement of tubes called stents in the oesophagus.
- If you had another test, like an upper gastrointestinal series of X-rays, and it showed abnormalities, you doctor will take a close look at the lining of the oesophagus with the esophagoscope.
How To Prepare For An Endoscopy of The Esophagus
Are you wondering about how to prepare for your upcoming endoscopy?
For an upper GI endoscopy, not a lot of preparation is necessary, though it is important to take note of the following:
- Fast For Four To Eight Hours Before. Because you would be having your upper gut and most times your stomach examined, it is important that your stomach is empty. You would in most cases therefore be required to have nothing to eat or drink for the last 4 to 8 hours before your procedure. Be sure to look out for the specific instruction your doctor would have given to you in this regard.
- Take All Your Usual Medications. If you are blood pressure pills, diabetes pills, or any other pill, be sure to take your medication (s) as usual even on the day of your esophagoscopy. If you are on a blood thinning medication, you could still take it in many cases, as long as your INR is within the required range. Sometimes though, your gastroenterologist would prefer you stop taking your blood thinning medications a few days before your procedure. Again, it is always best to confirm with your gastroenterologist, what he or she wants.
What To Expect After An Esophageal Endoscopy
In most cases, if you have not received a sedative or narcotics, the doctor will remove the endoscope and after a brief period of monitoring for complications, you will be discharged to your home.
You may have a sore throat, but it will resolve on its own, and you can begin to eat and drink normally within hours of discharge.
If you had sedation, you will be monitored in the recovery room until the sedatives or narcotics wear off and you are awake. Then, you will have a friend or family member drive you home.
It is important that you make arrangement for someone to take you home, as driving withing hours of having sedation could impair your reaction time and safety on the road.
Your doctor, the gastroenterologist, will visit the recovery area and tell you a little about what he did during the procedure and what he saw, but he will send the full report to your family physician, who will have an appointment with you to discuss any abnormal findings and to decide how to proceed.
References
- ASGE guidelines for clinical application. Establishment of gastrointestinal endoscopy areas. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. Dec 1999;50(6):910-2
- Principles of training in gastrointestinal endoscopy. From the ASGE. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. Jun 1999;49(6):845-53.
- Chan MF. Complications of upper gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. Apr 1996;6(2):287-303.
- Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. Jul 2007;66(1):27-34
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2871637/
Having An Esophageal Endoscopy Or Had One Already? Share Your Thoughts!
Are you waiting to have an esophagoscopy soon, or already had one? Do you have any question or perhaps comments? Is it about the interpretation of your result? Share your thoughts here. We would really love to hear from you!